More than 12.16 million cases of COVID-19 have been reported in the United States as of November 22, 2020. The toll of disease in the United States and globally is extensive and unprecedented by other illnesses in recent history. Global deaths are counted at nearly 1.38 million with the United States responsible for over 256,000 of these deaths.1 Clinical research, outcomes reporting, and innovation have focused on transmission of COVID-19 virus and management of moderate to severe COVID-19 disease. There is a growing interest in tracking outcomes and clinical innovation in managing patients with COVID-19 lingering symptoms or sequelae and identifying evidence-based treatment for patient with post-COVID syndrome.
Initial management of patients with COVID-19 takes place in one of three settings: 1) hospitals, 2) urgent care centers, and/or 3) ambulatory practices. Based on the COVID-19 experience at Northwell Health, New York’s largest integrated health care provider, recovery for the majority of patients will take place in the ambulatory setting, irrespective of the initial management setting.
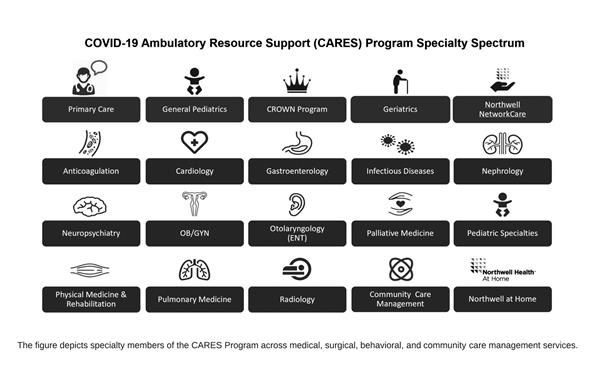
Thus, we created Northwell’s COVID-19 Ambulatory Resource Support (CARES) Program. There are various post-COVID-19 programs across the nation.2 Our CARES program is unique in that it is focused on offering a holistic approach to patients with post-COVID-19 symptoms and/or sequelae. It furthers the objective of building comprehensive expertise and collaboration between multiple specialties and clinicians to deliver patient-centered care.
The CARES Program is designed to be an interdisciplinary team representing the diverse group of experts and healthcare providers needed to care for patients with COVID-19. The CARES Program is comprised of two groups: a Steering Committee and Clinical Experts. Steering Committee members were intentionally chosen to represent frontline clinical experience in ambulatory and hospital settings, content expertise in COVID-19, patient navigation and care management experience, data and informatics expertise, and clinical and executive leadership. Clinical Experts were chosen through a process as follows:
The guiding principles for the CARES Program are straightforward: 1) each patient’s recovery is unique, and 2) continuous learning and improvement must be a focus, similar to the learning health system.3
Based on these guiding principles, we identified five core tenets of the CARES program:
- Leaning on the Patient-Centered Care model is key. This is a model of care that has been integrated into medicine, especially primary care, in recent years. This model advocates respect for patients’ desired clinical outcomes and their needs, whether they are focused on physical, emotional, social, or financial needs. Furthermore, patient-centered care emphasizes the importance of accessibility, collaboration, and coordination that would allow access to the right care, at the right time, and in the right place. The CARES program allows patients to choose their preferred providers, location, appointment day and time, and the setting in which they receive the care.
- Navigating patients to access care is important. With more than 22 hospital and 700 ambulatory practices, we decided it was important to create a model of care that navigates patients through the process of accessing care and beyond. We partnered with our nurse navigation team, Northwell NetworkCare, to allow patients to access care via a single-entry point: phone call to a toll-free number. Furthermore, clinicians can refer patients utilizing the electronic health record, where the order entry allows for multiple specialties to be chosen within a single order. Northwell NetworkCare nurses would subsequently triage patients for acute COVID-19 vs. post-COVID sequelae. Upon completion of intake, the nurse navigators would coordinate scheduling of appointments as well as post-appointment follow-up needs.
- Patient needs are varied and access to experts needs to equally wide ranging. The sequelae of COVID-19 are wide ranging, from semi-acute to chronic, including fatigue, myalgias, myopathy, vasculitis, anxiety, depression, and neurological changes such as cognitive decline, to name a few. The same symptoms have been described in the recovery from mild COVID-19 illness.4, 5 Furthermore, the persistent symptoms and delayed recovery are not the only COVID-19 sequelae. It is hypothesized that among patients and families recovering from COVID-19, the burden of social determinants of health has significantly increased. Also, the community and care management needs of patients recovering from COVID-19 are significant. Thus, we wanted to include experts across a wide range of medical, surgical, and behavioral specialties. We asked the respective leaders at Northwell Health to identify COVID-19 ambulatory experts in their specialties, practices, and programs (see figure).
- Access to care needs to be across the geographic footprint. Northwell Health is a large integrated system with a diverse patient population and it serves multiple counties in New York including: Suffolk, Nassau, Queens, Brooklyn, Manhattan, Staten Island, and Westchester. Upon identifying needed specialties, the next step was to ensure we had access to experts across the footprint. In areas where expertise was physically available in a timely manner, telehealth technology was leveraged when appropriate and preferred to expedite access to clinical expertise. Furthermore, our partnership with home care allows patients to access care in multiple settings: at office, in person, telehealth, and home-based.
- Clinical expertise needs to be built in a collaborative and continuous manner. Current understanding of post-COVID sequalae is quite limited. Thus, the CARES program is focused on continuously building our expertise in managing post-COVID sequelae. To aid in continuous learning, the CARES program features a virtual collaboration platform for the previously mentioned COVID-19 clinical experts called the Learning Collaborative. This is a biweekly virtual meeting featuring discussion on post-COVID cases and newly published evidence in diagnosis, management, or mitigation of post-COVID sequelae. In addition, program services and offerings are routinely reviewed to disseminate up-to-date information on the CARES Program.
The majority of patients with COVID-19 will continue their diverse, and at times challenging, journeys to recovery in the ambulatory setting. Northwell Health’s experience with the management of COVID-19 is consistent with this, regardless of whether initial diagnosis and management happened at home or in a hospital setting. Given limited studies of the prolonged recovery from COVID-19, we anticipate that the CARES program will offer unique insights related to long-term effects of COVID-19 on physical, emotional, social, and overall wellness recovery. Future studies will be focused on detailed evaluation of the program, enrolled patient characteristics, patient and clinician satisfaction of program, and more. Post-COVID recovery is a new process and we have yet to understand the view of COVID-19 recovery 1, 5, and 10 years from now.
For further information on CARES, refer to this site: www.Northwell.edu/CARES.